

Andréa Santos Soares1; Ana Paula Dornelles Manzoni2; Carla Daniele Amorim de Souza3; Magda Blessmann Weber4; Tatiane Watanabe1; Leandra Camini5
Introduction: Although the intradermal melanocytic nevi are benign lesions, many patients seek for dermatologists for their excision. However, there are no studies about the best method for this procedure.
Objective: To compare in a randomized clinical trial the excision of intradermal melanocytic nevi in the face for shaving and elliptical excision with suture
Methods: Patients with intradermal melanocytic nevi on the face were selected for removal by shaving or ellipse, randomly. The results were described regarding patient satisfaction and photographic records evaluated by a blinded physician.
Results: 18 patients underwent excision of intradermal melanocytic nevi. The mean scar size after six months of the procedure was of 8,11mm for the excision in ellipse and 2,92mm for the shaving (p < 0.05). The mean score of the patients after six months was 9.67 (ellipse) and 9.57 (shaving) (p = 0.8). The mean by the blinded physician was of 7.78 (ellipse) and 7.86 (shaving) (p = 0.91). 28.6% of patients undergoing shaving had recurrence of the nevus.
Conclusions: The two forms are of excision are equivalent concerning patients satisfaction and the judgment of medical team about the aesthetic results of the scar. However, ellipse with suture excision has the advantage of having a lower relapse.
Keywords: NEVUS, INTRADERMAL; AMBULATORY SURGICAL PROCEDURES; SKIN; THERAPEUTICS
Acquired melanocytic nevi are benign lesions originated from melanocytes, and can be classified as junctional, compound or IMN. 1.2 The progressive decrease in its growth rate and the emergence of differentiation of cells in melanocytic nevi lend the benign characteristic to the lesion, which are generally solid and can vary in size. 1 IMN (IMN) are nevi with little presence or absence of melanocyte proliferation in the epidermis, and its main characteristic is the presence of clusters of nevus cells in the dermis. 1 The cells that are located more deeply in the dermis tend to assume neuroid or fibroblastic morphology, and lose their melanin synthesizing capacity, meaning that the vast majority of IMNs are clinically not pigmented. 1 The diagnosis of IMN is usually clinical, and its malignization risk is low. 1 On examination, the lesions appear to be papular, normochromic or slightly pigmented, 1.2 and are most commonly found on the face. Telangiectasias and terminal hairs may be present. 1 Differential diagnosis of IMN includes dermatofibromas, neurofibromas, fibroepithelial polyps, and basal cell carcinomas, among others. 2
The excision of IMN is indicated when there are proven clinical or dermoscopic changes and atypical appearance of the lesion, nevertheless they are more often excised due to aesthetical reasons or repeated local traumas. 2
Currently, there is no consensus on the best way to excise an IMN, and it is up to the dermatologist to use the shaving technique or the elliptical excision followed by suture.
Shaving – or saucerization – is the removal of the lesion by cutting its base parallel to the skin, using a scalpel or scissors. Elliptical excision corresponds to the ellipse-shaped exeresis of the skin around the lesion. It allows the removal of all skin layers up until the hypodermis and requires suturing. The present study was aimed at comparing the two procedures regarding the patients' and dermatologist physicians' satisfaction with the aesthetic results, and the lesion's risk of recurrence.
A comparative randomized clinical trial, blind to an observer, was carried out at the Dermatology Service, Universidade Federal de Ciências de Saúde de Porto Alegre (UFCSPA), Porto Alegre, Brazil, including 18 patients with clinical diagnosis of IMN on the face, from August 2014 to June 2015. The study was approved by the Research Ethics Committees of both UFCSPA and the health center Santa Marta (Porto Alegre, RG, Brasil).
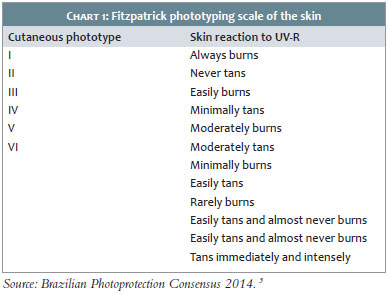
Patients of both genders bearing intradermal nevi diagnosed based on the classical clinical manifestations (normochromic melanocytic papular lesions) and dermoscopic characteristics (focally located globules or structures similar to globules, whitish areas without structure, and thin linear vessels or in the shape of a comma), located on the face, which corresponds to the area of ¿¿highest prevalence of IMN. Patients were aged between 18 and 80 years, had Fitzpatrick's phototypes I to IV (Table 1), and accepted to take part in the study by signing the Term of Free and Informed Consent. Patients whose nevi had undergone previous procedures, those with undiagnosed or poorly controlled clinical diseases (for example diabetes, Thyroiditis, hypertension), previous history of Keloid, use of medications that alter wound healing (eg. isotretinoin and immunosuppressants), were exclusion factors. Also, patients who did not follow the evaluation schedule or who did not have confirmation of the clinical diagnosis by histology after undergoing exeresis of the lesion were excluded.
The patients were alternately selected to undergo shaving or excision, followed by suture, observing the order of inclusion in the study. The lesions that had been randomized to undergo for ellipse exeresis (always observing the skin's tension lines for better incision and suture) were demarcated so as to maintain a 30º angle at the ellipses' borders, restricting the incision's length to three times the width's length, maintaining a margin of 1mm to 3mm from the intradermal nevus. Sutures were performed with separate single stitches, using a 6/0 nylon thread. Micropore was applied on the suture, with patients being instructed to remove it after 24 hours, and carefully cleanse the surgical wound once day with water up until the stitches have been removed in the 7th post-operative day, at UFCSPA's Dermatology Service.
The lesions that were randomized for the shaving procedure underwent excised by the means of an incision carried out at the base of the lesion, flush to the skin, using a scalpel blade number 15. The hemostasis was performed only with local compression. Micropore was applied on the site and the patients were instructed have it removed 24h after, with gentle cleansing with water once a day. All surgical procedures and advice were given to the patients by the same dermatological surgeon on all follow-up visits.
Regarding the patient follow-up visits, all were contacted 48h after the procedures for the classification of the intensity of discomfort with the excision. This classification was based on an analogue scale of pain graded from "zero" (absence of discomfort) up to "10" (unbearable discomfort), with the patients being advised that "discomfort" would include the presence of pain, bleeding, restriction to movement, and difficulty to sleep.
The patients returned to the UFCSPA's Dermatology Service after 3 and 6 months of the procedure for postoperative evaluation and having their surgical wound photographed. Pre-and post-procedure photographs were taken under standardized environmental, lighting, and technical parameters (including the camera and the photographer), and the lesion was measured in millimeters before the procedure and at all subsequent visits. All patients were instructed to use sunscreen with at least SPF30 (reapplied each 4 hours), in addition to physical protection for at least 6 months.
Regarding the statistical evaluation, the qualitative data were assessed using frequency and percentage analysis, while the quantitative data were assessed based on mean values and standard deviation (when normally distributed) and median and interquartile range (when the distribution was not normal). The data normality was verified using the Shapiro-Wilk test. The comparisons between the different types of treatment were performed using the Fisher exact test (qualitative variables), the Student's t-test (normally distributed quantitative variables) and the Mann-Whitney test (non-normally distributed quantitative variables). The comparisons between the assessments performed by the physician and the patient were analyzed by using the Student's t-test, according to the assessment timepoint and the treatment. The data were recorded on an electronic spreadsheet and analyzed using the software SPSS V21A. The statistical significance was 5% (p-value < 0.05).
Eighteen patients with lesions on the face underwent excision of IMN. The histological analysis revealed the following diagnoses: IMN (16 cases, 88.9% of the sample cases); compound melanocytic nevus (1 case) and hemangioma (1 case). As a result, 11.5% of the facial lesions had discordant histological and clinical diagnoses. These patients were excluded from study.
The analyzed sample had 16 patients (2 men, 14 women). The profile of the patients included in the study is described in Table 1, evidencing the sample homogeneity regarding the patients' age, gender and phototype. Patients were followed-up for up to 6 months.
The average IMN size studied was 3.94mm for those excised with the elliptical technique, and 3.92mm for those excised using the shaving technique. The sample was homogeneous for all groups described (Table 1).
The average scar size after 6 months was 8.11mm for lesions excised with the elliptical technique, and 2.92mm for those excised with the shaving technique (p <0.05), as seen in Table 2. In the evaluation performed 6 months after the procedure, the mean rating attributed by the patients regarding the procedure's final outcome was 9.67 for those who underwent fusiform (elliptical) excision and 9.57 for those who underwent the shaving procedure (p = 0.8). Regarding the evaluation performed by the blinded physician, the average rating regarding the procedure's final outcome was 7.78 for the patients undergoing fusiform (elliptical) resection and 7.86 for those who underwent shaving exeresis (p = 0.91) (Table 3).
Only two patients reported discomfort after the procedure (attributing the rating "1" on a scale from "zero" to 10), with each of them belonging to one of the groups (elliptical excision and shaving procedure) (Table 2).
None of the patients developed hypertrophic scarring or keloid during the follow-up period the procedure. Regarding the recurrence of the lesion after the procedure, none of the patients who underwent fusiform (elliptical) excision experienced recurrence while 28.6% of those ho underwent the shaving procedure in the same group had recurrence (Table 2).
There is lack of scientific literature effectively comparing options and indicating the best treatment for IMN. Some studies evaluate the durations of the healing, bleeding and infection, however there are no studies comparing the shaving technique with fusiform excision followed by suture.
Histological analysis in the present study evidenced that 88.9% of the lesions excised were IMN, as previously clinically diagnosed. The discordant cases were: one compound melanocytic nevus and one hemangioma. This fact shows a high level of agreement between the histology and the clinical manifestations of IMN, nevertheless it highlights the paramount importance of submitting all excised lesions to histological examination. In the present study, all discordant lesions were benign, however differential diagnoses, such as amelanotic melanoma and basal cell carcinoma, should not be overlooked. 2.4
In the present study, the scars from lesions excised via the shaving technique were significantly smaller than those excised using fusiform excision (Figures 1 and 2) – and even smaller than the lesions before undergoing the procedure (Figures 3 and 4) (p <0.05). The outcomes corroborate the literature findings, which state that approximately 45% of the facial nevi excised using the shaving technique generate scars that are smaller than the original lesions. 1 The smaller size of the scar as compared to the initial nevus lesion after shaving excision is possibly due to the cicatricial retraction of the tissues. On the other hand, the fusiform (or elliptical) technique requires that the length of the surgical piece be roughly three times larger than the nevus, which leads to an increase of the scar in this technique. 1
All patients included in the study (in both groups) were very satisfied with the procedures' outcomes. The difference between the average rating for the patients' satisfaction with the shaving technique and with exeresis followed by suture was little, with a slightly greater satisfaction with the elliptical excision, however without statistical significance (p = 0.8). In their study, Lee et al. also demonstrated a significant patient satisfaction index associated to the shaving technique used for the removal of IMN. 5
In the present study, none of the patients developed hypertrophic scar or keloid during the follow-up period. This may be linked to the fact that patients with lower phototypes (II and III) were selected, in addition to the small size of the studied sample. 6
It was possible to observe a low recurrence rate linked to the excision of facial lesions using the shaving technique. It is known that the most superficial excision caused by the shaving technique increases the risk of recurrence of the nevus as compared to the excision up until the hypodermis followed by suture. Nonetheless, the real reason for the recurrence and its correlation with that technique needs to be better studied.
It is possible to conclude that the two excision techniques are equivalent in terms of patient satisfaction and the rating attributed by the medical team to the esthetical outcomes of the scar. Nevertheless, the fusiform (or elliptical) exeresis has the advantage of having a lower recurrence rate. Despite the results that were obtained, more studies are necessary aimed at consolidating the present paper's findings.
1. Burns T, Breathnach S, Cox N, Griffiths C. Rook's Textbook of Dermatology. 8th ed. Oxford: Wiley-Blackwell; 2010.
2. Bolognia JL, Jorizzo JL, Schaffer JV. Dermatology. Rio de Janeiro: Elsevier; 2015.
3. Schalka S, Steiner D, Ravelli FN, Steiner T, Terena AC, Marçon CR, et al. Consenso Brasileiro de Fotoproteção. An Bras Dermatol. 2014;89(6 Suppl 1):S6-75.
4. Arjona-Aguilera C, Gil-Jassogne C, Jiménez-Gallo D, Albarrán-Planelles C. Intradermal Melanoma Associated With an Intradermal Melanocytic Nevus. Actas Dermosifiliogr. 2015;106(9):776-7.
5. Lee JM, Lee H, Lee TE, Park M, Baek S. Second intention healing after shave excision of benign tumors on the lid margin. Ann Dermatol 2011;23(4):463-7.
This study was carried out at the Dermatology Department of the Universidade Federal de Ciências de Saúde de Porto Alegre - Porto Alegre (RS), Brazil.